WHY ASK ABOUT SEXUAL ORIENTATION AND GENDER IDENTITY?
There is a growing body of evidence showing that Lesbian, Gay, Bisexual, Transgender, and Queer/Questioning (LGBTQ+) youth suffer from potentially traumatic events (PTEs) at significantly higher rates than their straight and cisgender peers. Among the most prevalent PTEs affecting LGBTQ+ youth are parental rejection, bullying, physical and sexual harassment, and hate crimes. Consequently, LGBTQ+ youth experience a wide array of health disparities, such as increased rates of anxiety, depression, suicidal ideation and attempts, drug and alcohol misuse, sexually transmitted diseases/infections, homelessness, and Post Traumatic Stress Disorder (PTSD). The alarming rate at which LGBTQ+ youth are victimized in the United States urges us to identify LGBTQ+ youth in order to assess for safety and risk of self-harm or suicidality, prevent exposure to trauma via psychoeducation, and refer to evidence-based trauma-focused treatment when they have been exposed to trauma. Nevertheless, discussing and acknowledging sexual orientation and gender identity—with or without the aforementioned PTEs—has not been common practice in child-serving systems and organizations.
Often LGBTQ+ youth’s increased risk for trauma is partly due to societal stigma and prejudice. As a trauma treatment provider, you have an obligation to provide safe and affirming spaces for LGBTQ+ youth to express themselves honestly—without fear of judgment, ridicule, or having their identities outed. Additionally, you must ask about essential and basic information such as gender identity, sexual orientation, and PTEs. Without asking these important questions, you cannot provide trauma-informed services that truly meet the unique needs of LGBTQ+ youth and their families. It is essential that as a provider, you actively acknowledge and validate youth who hold marginalized identities and seek to understand the ways in which these identities and PTEs may intersect.
Share This Post!
Emotional and Psychological Trauma
By Lawrence Robinson, Melinda Smith, M.A. and Jeanne Segal, Ph.D. What is emotional and psychological trauma? Emotional and psychological trauma occurs when extraordinarily stressful events shatter your sense of security. Psychological trauma can leave you [...]
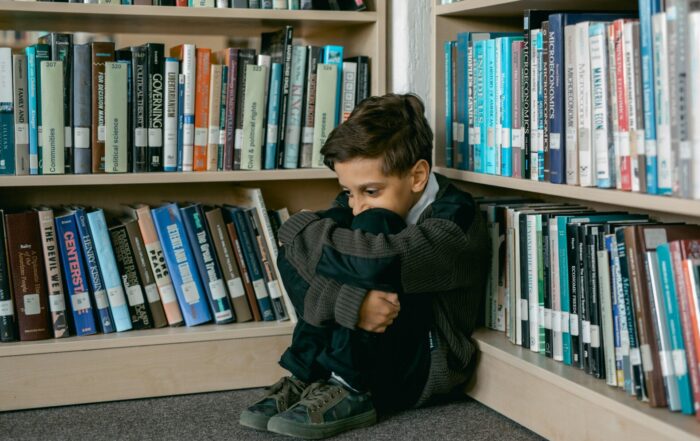
Understanding Childhood Trauma: Ways to Support Young People
By Boys & Girls Clubs of America For generations, tough childhood experiences have been swept under the rug by phrases like these. Oftentimes, the reason why is simple: many families simply did [...]
Addressing The Link Between Trauma And Addiction
By National Governors Association Many Americans have experienced traumatic events, toxic stress, and other types of adversity in childhood. However, repeated exposure to trauma and adversity in childhood predicts a variety [...]
The Health Benefits of Volunteerism
By Eric Burger It’s a simple fact that every nonprofit organization knows: volunteering makes you feel better. But did you know that the anecdotal stories about volunteering health benefits have been [...]
Checklist: Creating Safe Spaces for Youth
By Mental Health America Now more than ever, young people need an environment where they feel seen, heard, and valued. [...] Creating connection starts with you, so allow youth to get [...]
What is Childhood Trauma: Trauma Types
By The National Child Traumatic Stress Network When a child feels intensely threatened by an event he or she is involved in or witnesses, we call that event a trauma. There [...]